Mr Nick Savva FRCS & Mr Heath Taylor FRCS Consultant Orthopaedic Surgeons, Specialists in Foot & Ankle Surgery
www.taylorsavvamedicolegal.co.uk
Arthritis is a degenerate joint condition that occurs commonly as part of the normal ageing process. The risk of arthritis is increased in patients that suffer injury around joints. This can occur either by direct injury to the joint surface itself, or by injury to the bones around the joint, causing mal- alignment and altering the joint mechanics.
A normal synovial joint, such as the knee or ankle, is a complex structure that allows pain free, low friction movement. It relies on the joint surfaces being a perfect fit for one another (congruence) as well as a low friction lining (cartilage).
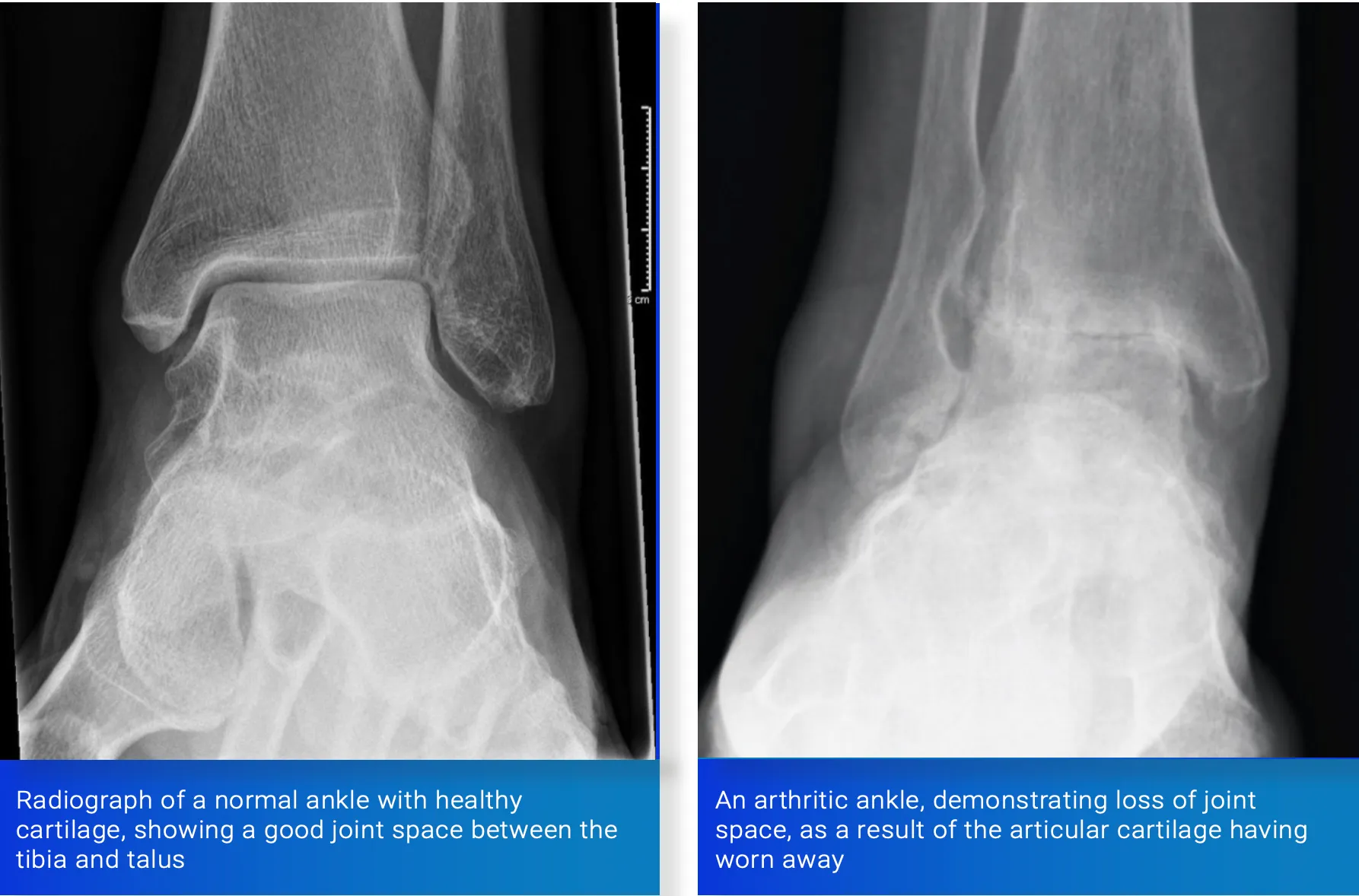
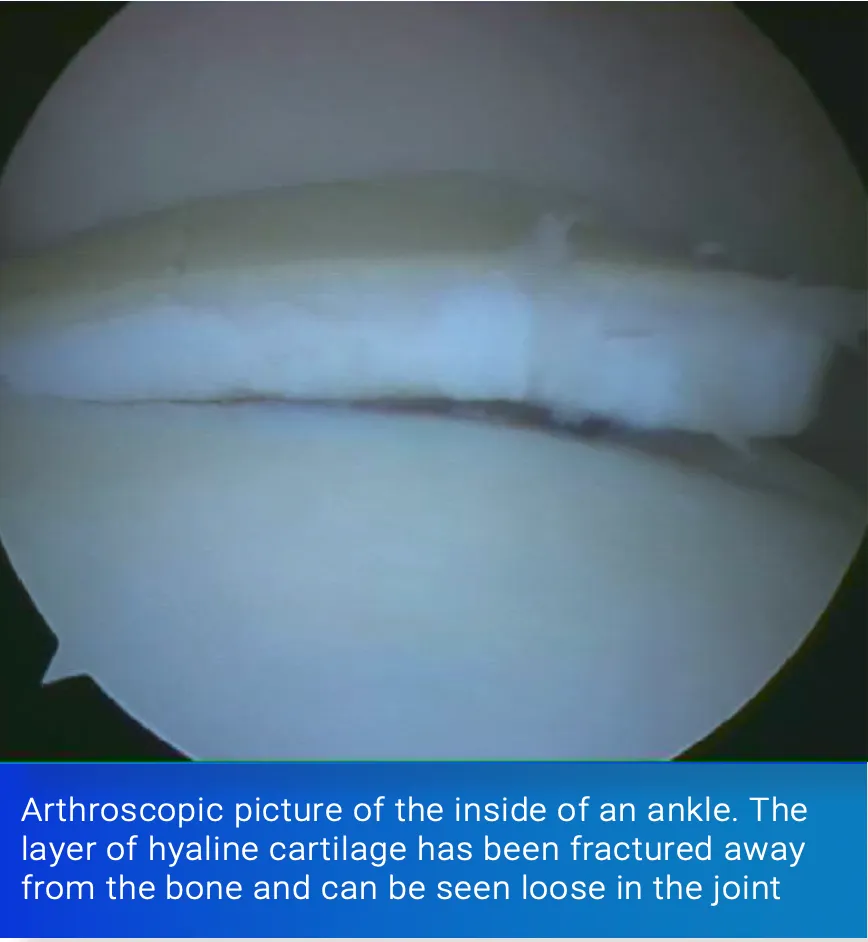
The hyaline cartilage that lines a synovial joint is a highly specialised substance with unique properties. It has a very low coefficient of friction, allowing smooth joint movement. The body is unable to produce hyaline cartilage and repairs injury with fibrocartilage. This is a less resilient, higher friction form of cartilage not usually found in synovial joints and as a result is less effective in facilitating joint glide.
Post traumatic arthritis is a form of arthritis caused by injury. There are a number of factors to be taken into account when assessing the risk of developing arthritis.
1) Indirect Trauma to the Joint Surface.
When a long bone such as the tibia is broken in an accident, the joints at either end can also absorb a significant amount of the energy. This may not be enough to show on plain x-ray or MRI scan, but can manifest as arthritis later in life. Subtle clues, such as painful swollen joints at the time of injury are often missed or overlooked, owing to treatment being concentrated on the main injury.
2) Intra-Articular Fractures.
Intra-articular fractures occur when a large amount of force passes through a joint. Such a fracture may breach the bone and cartilage of the joint. This results in irregularities or even steps in the hyaline cartilage. These fractures can either be undisplaced and amenable to non-operative treatment or displaced, in which case surgery may be considered.

The risk of post-traumatic arthritis is particularly increased when the joint surface heals in a non-anatomical position. This can alter the biomechanics of the joint. Irregularities and steps in the cartilage predispose to arthritic change, although the height of step that is significant is difficult to estimate, and varies joint by joint. Evidence around this subject is contentious. A good rule of thumb is that if the step is greater than the thickness of cartilage in the joint, the outcome is likely to be unfavorable.
When assessing the risks of a patient developing post-traumatic arthritis after an intra-articular fracture, particular attention is paid to the degree of comminution at the fracture site. This is the number of fracture fragments that are present - the greater the number, the higher the force applied and the greater the potential damage to the joint surface, resulting in an increased risk of the development of arthritis.
3) Open (Compound) Fractures, Resulting in Infection within the Joint - Septic Arthritis
The results of septic arthritis in uninjured joints are often poor, as the common bacteria that cause this condition release toxins that damage cartilage. The most effective treatment is prompt surgical wash out of the joint and appropriate antibiotics.

A compound intra-articular fracture is a fracture that occurs in a joint, with an overlying breach in the skin and soft tissues. These injuries have a high risk of infection, and urgent surgical debridement and antibiotic treatment are required. The results of septic arthritis can be devastating, with high risks of poor outcome or arthritis. Occasionally, severe infection that cannot be eradicated may necessitate amputation. Treatment for such conditions is likely to be protracted, with poor long-term outcomes.
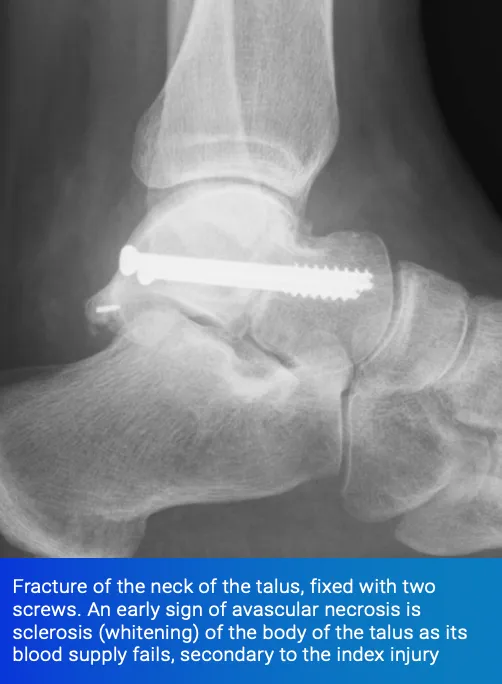
4) Damage to the Blood Supply - Avascular Necrosis
Certain fractures are renowned for damaging the blood supply of the bone. Common examples are fractures of the hip and fractures of the talus, the main bone in the ankle joint.
Talar neck fractures, if caused by a high-energy injury with significant displacement, can completely disrupt the blood supply to the body of the talus. This can cause the bone to die and collapse, resulting in arthritis and may necessitate salvage procedures such as fusions around the hindfoot.

5) Mal-Alignment of a Joint Due to Distant Fracture
The forces passing through a joint are balanced to equalise pressure on the cartilage. If a fracture heals in a non-anatomical position, this can alter the delicate balance, resulting in early arthritis of the joint. For this reason, great care is given, when stabilising long bone fractures, to ensure correct alignment is restored.

6) Chronic Instability of a Joint
Joint motion is stabilised and limited by ligaments. These ensure that the joint stays within its physiological range and avoids overload on the hyaline cartilage.
Injuries can cause rupture of the ligaments and result in joint instability. This can be a disabling problem in its own right requiring bracing, physiotherapy or reconstructive surgery.
Good examples include the lateral ligaments of the ankle and the anterior and posterior cruciate ligaments of the knee.
Chronic instability, such as can occur in patients that suffer significant ankle injury, can cause repetitive injury to the joint, resulting in eventual damage to the articular cartilage.

7) Other Causes of Joint Injury
Injuries to other structures in a joint, such as the menisci, or shock-absorbing cartilage, in the knee, or the labrum in the hip can alter joint mechanics, resulting in the development of arthritis in the future.
Summary
In summary, the causes of arthritis after injury are multiple and all must be taken into account when calculating the risks of the development of arthritis after injury. In particular, the degree of intra-articular injury, combined with the force applied and amount of comminution are important when assessing the risk, as they all directly impact on the amount of cartilage damage sustained.
Mr Nick Savva FRCS & Mr Heath Taylor FRCS
Consultant Orthopaedic Surgeons Specialists in Foot & Ankle Surgery www.taylorsavvamedicolegal.co.uk
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
Unordered list
Bold text
Emphasis
Superscript
Subscript