By Dr Michael D Spencer MA, MD, MB BChir, FRCPsych
Consultant Psychiatrist, Cambridgeshire and Peterborough NHS Foundation Trust; Honorary Consultant Psychiatrist, Pain Management Centre, University College London Hospitals NHS Foundation Trust
Further information and contact details: mdspencer.com | psychiatry-expert.com
Introduction
The intersection of post-traumatic stress disorder (PTSD), chronic pain, and personal injury presents a complex landscape with significant implications for both medical treatment and the medicolegal process. Understanding how these conditions interact and influence each other is essential for experts to provide accurate and evidence-based advice to the Court in chronic pain cases. This article provides an introduction to the intricate relationships among these factors, examining how chronic pain and PTSD are intertwined with personal injury litigation and the implications for treatment strategies.
Relevance of the Intersection
Chronic pain and litigation have been cited as risk factors for promoting adverse outcomes in PTSD. Similarly, PTSD and litigation are recognised as factors that can negatively impact the outcomes of treatments for chronic pain conditions, such as neuromodulation (Gatchel et al., 2007). This raises the question of whether PTSD and/or chronic pain can improve or respond to treatments during litigation, or whether treatment should be postponed until after a legal settlement is reached. The reality, however, is more nuanced.
Chronic pain and PTSD often coexist, creating a bidirectional relationship where each condition can exacerbate the other. PTSD symptoms are common in individuals with chronic pain, with various large studies reporting between 10 – 50% of patients referred for chronic pain rehabilitation as meeting diagnostic criteria for PTSD (Asmundson et al, 2002; Andersen et al, 2012; Andersen et al, 2014). Similar variation in the prevalence of chronic pain symptoms has been reported in individuals with PTSD, with rates between around one-third to two-thirds - although research has largely involved veteran rather than civilian populations (Beckham et al, 1997; Shipherd et al, 2007).
Chronic pain can serve as a constant reminder of the traumatic event, triggering PTSD symptoms and leading to heightened pain sensitivity. Conversely, PTSD-related hyperarousal and anxiety can amplify the perception of pain, creating a vicious cycle of mutual maintenance, that complicates both conditions (Sharp and Harvey, 2001; Asmundson et al., 2002; Jenewein et al, 2009). A number of studies have indicated that the presence of PTSD symptoms has an adverse impact on the course of chronic pain complaints following injury such as whiplash, being associated with a more severe and persistent pain presentation (Buitenhuis et al, 2006; Sterling et al, 2006); and in turn that more severe pain and disability is correlated with a more persistent course of PTSD symptoms (Ravn et al, 2019; Giummarra et al, 2017).
Figure 1 illustrates the process whereby the mutually maintaining interactions between psychological trauma and chronic pain can promote a cycle of chronic pain, PTSD, and avoidance behaviour, leading to increasing disability and distress.
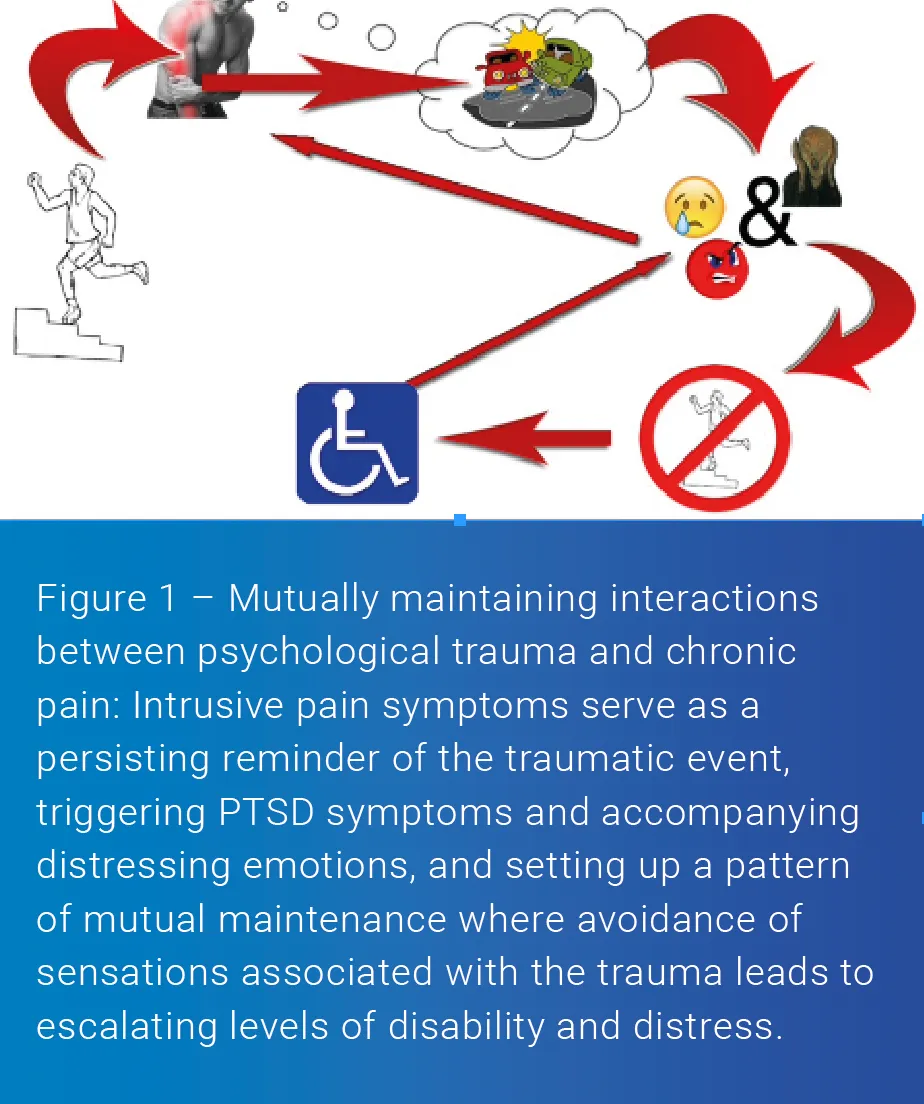
Psychological factors play a crucial role in linking chronic pain and PTSD. Anxiety, hypervigilance, and trauma-focused cognitive processes can amplify pain perception, while maladaptive coping strategies, such as avoidance and catastrophising, can sustain both conditions (Vlaeyen & Linton, 2000). Perceived injustice and catastrophisation have been shown to play important roles in sustaining both PTSD and pain symptoms following physical injuries such as whiplash injury (Sullivan et al, 2011; Sullivan et al, 2012; Andersen et al, 2016). Understanding these mechanisms is essential for developing effective treatment strategies that address both the psychological and physical aspects of these conditions.
Neurobiological studies suggest that chronic stress and hyperarousal associated with PTSD can alter pain thresholds and pain processing pathways, leading to increased pain sensitivity and chronicity (Defrin et al., 2008). The interplay between the central nervous system's response to pain and stress underscores the importance of integrated treatment approaches that address both PTSD and chronic pain.
Impact of Litigation on PTSD and Chronic Pain
Personal injury litigation introduces additional stressors with the potential to exacerbate both PTSD and chronic pain. The adversarial nature of the legal process, the requirement to repeatedly recount traumatic events, and the uncertainty of legal outcomes can all serve as significant stressors with the potential to exacerbate the symptomatology of these conditions. A sense of not being believed may also represent a stressor – and as Hickling et al (2006) commented, “Patients as participants in this process may come to see that even though they see themselves as the victims, they are now the ones placed on trial, exacerbating their sense of vulnerability and victimization.” However, it is important to recognise that discussing trauma memories is not necessarily “re-traumatising” (Murray et al., 2022). While many individuals may experience distress when talking about their trauma memories, and some might experience a temporary, modest symptom exacerbation afterwards, research in trauma-focused CBT (TF-CBT) suggests that engaging with, rather than avoiding, trauma memories through talking and/or writing is one of the most effective elements of treatment (Shearing et al., 2011).
Involvement in litigation has been associated with elevated distress and slower recovery among patients with PTSD (Blanchard et al., 1998; Frueh et al., 2003), greater levels of pain and disability (Tait et al., 1990), and poorer outcomes following spinal surgery (Epker and Block, 2001; Harris et al., 2005).
On the other hand, Mayou and colleagues reported that involvement in litigation did not predict any aspect of psychological outcome at one year following a road traffic accident (Mayou et al, 1993), whilst Bryant and Harvey reported that settlement of compensation claims following motor vehicle accidents did not influence reported PTSD symptoms (Bryant and Harvey, 2003). Andersen and colleagues found that patients can still benefit from multidisciplinary chronic pain rehabilitation despite the presence of comorbid PTSD (Anderson et al, 2014).
A systematic review of 29 prospective cohorts of patients with whiplash-associated disorder (WAD) found that litigation was not a predictor of outcome (Scholten-Peeters et al., 2003). More recent studies have indicated that individuals with active litigation can experience improvements in emotional distress, pain intensity and return-to-work status following interdisciplinary pain management programs (Gagnon et al., 2013); furthermore, clinically significant improvements in pain measures have been reported following a UK-based multidisciplinary pain management program, even among individuals involved in litigation (Twiddy et al., 2019).
Thus, whilst the literature points to associations that underscore the potential for litigation to negatively impact both psychological and physical health outcomes, the relationship between litigation and health outcomes is complex and not universally negative; and while litigation can introduce stressors that potentially exacerbate PTSD and chronic pain, effective treatment strategies can still be beneficial.
Additionally, there is evidence suggesting that individuals involved in litigation can still benefit from treatment for PTSD, supporting the notion that litigation should not serve as an exclusion criterion for psychological intervention (Shorer et al., 2021). This perspective aligns with the NICE guidelines on the management of PTSD (National Collaborating Centre for Mental Health, 2005), which recommend that “Healthcare professionals should not delay or withhold treatment for PTSD because of court proceedings or applications for compensation” – thus emphasising the importance of providing timely and appropriate care to individuals with PTSD, irrespective of their involvement in litigation.
Neuromodulation and Psychological Assessment
In the realm of neuromodulation for chronic pain, there has been a significant shift from viewing psychological assessments as gate-keeping mechanisms designed to exclude patients with “red flags”, to an approach that emphasises the role of the psychologist and/or psychiatrist in supporting the patient and the multidisciplinary team, and contributing to multimodal prehabilitation. This shift recognises the importance of providing treatment at the right time and focuses on improving measurable psychosocial factors - such as “patient activation”, which refers the “extent to which patients are engaged and active in their own health care” (Hibbard et al, 2004). Recent research indicates the role of increased patient activation in mediating positive outcomes from spinal surgery, even where adverse psychosocial risk factors are present (Block et al, 2019).
Thus, whilst ongoing litigation has been associated with poorer outcomes following spinal surgery, recent advances in the practice of psychologically-informed prehabilitation, multidisciplinary working and our understanding of how to support patients with psychosocial risk factors such as psychological trauma and ongoing litigation does highlight the need for research to inform guidelines on the management of these complex cases.
Conclusion
The intersection of PTSD, chronic pain, and personal injury litigation presents a complex and challenging landscape for both medical and legal professionals. Understanding the intricate relationships among these factors highlights the intertwined nature of chronic pain and PTSD, and is essential for experts to provide accurate and evidence-based advice to the Court in chronic pain cases.
Scan the QR-Code below to view the full list of references

Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
Unordered list
Bold text
Emphasis
Superscript
Subscript